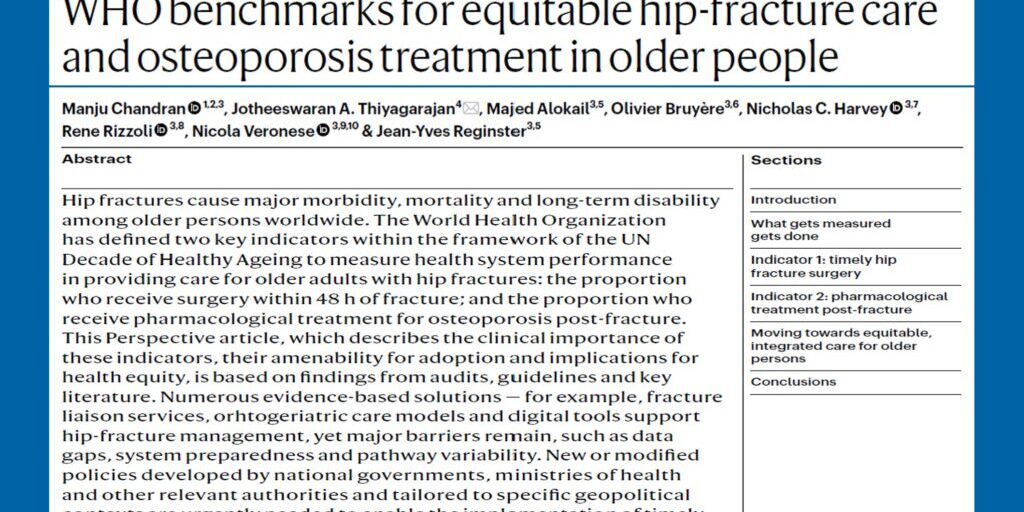
The Asia Pacific Consortium on Osteoporosis (APCO) unites clinical experts from across our region to develop practical solutions to pressing challenges facing osteoporosis management and fracture prevention in this highly populous region of the world. It is important that we monitor the evolving global osteoporosis landscape and consider its potential impact on practice here in the Asia Pacific region.
The last year has seen updated osteoporosis guidance and guideline documents published by the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO)/International Osteoporosis Foundation (IOF) and the Endocrine Society, and last month the American Association of Clinical Endocrinologists (AACE) and the American College of Endocrinology (ACE) updated its clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis.
The executive summary highlights the 52 recommendations made, of which 84% are Grade A or B. The evidence-based guidelines provide “nuance-based clinical decision-making that addresses multiple aspects of real-world care of patients”.
One area of interest, in which it aligns to a position paper published jointly by the ESCEO and IOF , AACE/ACE provide practical recommendations to stratify patients into high risk or very high risk. All individuals with a FRAX (or if available, TBS-adjusted FRAX) 10-year probability for major osteoporotic fracture of ≥20% or the 10-year probability of hip fracture of ≥3% are recommended for pharmacological therapy, even if BMD is in the “osteopenic” range. “Very high risk” individuals are those with a recent fracture; fractures while on approved osteoporosis therapy; multiple fractures; fractures while on drugs causing skeletal harm; very low T-score (e.g., <-3.0); high risk for falls or a history of falls, and a FRAX probability for major osteoporosis fracture >30%, or hip fracture >4.5% over a 10-year period.
Of note, each guideline provides subtly different criteria, with the ESCEO/IOF position paper applying age-specific thresholds to define high versus very high risk.
So, what does this mean for practice in Asia-Pacific?
With the changing landscape of pharmacological options and consideration of the lifetime osteoporosis journey, clinicians may benefit from practical guidance on treatment choices. Those at higher risk require more potent therapies, and for those at lower risk, we need to decide whether pharmacological therapy has a role to play or not.
Stratification of osteoporotic fracture risk to guide treatment choice (or a decision not to treat) is clearly gaining traction globally. At a regional and national level, professional societies and guideline authors will need to review these recommendations, to determine the relevance to their local practice and whether the “nuanced” advice offers tangible benefits to their peers.
Some challenges to implementation across Asia would need to be considered: firstly, the authors of the AACE/ACE guidelines state that the FRAX thresholds they apply are US-specific and that country-specific thresholds should be applied. While the FRAX tool has been validated in many Asian countries, in addition to intervention tools such as the Garvan, which is also employed in Australia, most Asian countries have not implemented specific intervention thresholds for use yet.
Furthermore, recommendations need to consider local reimbursement criteria, which often dictate eligibility criteria for pharmacological treatment options.