Use of NHANES III reference range for bone mineral density (BMD) can result in an overdiagnosis of osteoporosis in Asians
The diagnosis of osteoporosis is operationally based on a measurement of bone mineral density (BMD), preferably at the femoral neck or total hip. According to WHO’s recommendation, osteoporosis is defined as a BMD T-score of -2.5 or lower at the femoral neck. This threshold of -2.5 was actually a compromise of prevalence, clinical association and subjectivity (e.g. “we know it is true” versus “we know it is not true”). It was chosen so that the prevalence of osteoporosis is equivalent to the lifetime risk of fracture among Caucasian women, which is about 30%.
Although the concept of T-score was heavily criticized as a flawed approach, it is widely used in clinical practice to make a diagnosis and initiate treatment of osteoporosis. Statistically, T-score is calculated from the mean and standard deviation of BMD measurements derived from a reference population aged 20-29 years (i.e. peak BMD). The International Osteoporosis Foundation (IOF) recommended use of the NHANES III data as a reference range for the diagnosis of osteoporosis for all populations.
However, BMD is known to differ between ethnic populations, and the difference is not due to artificial factors. For example, among pre-menopausal women, Afro-Caribbeans have higher BMD than Caucasians, who in turn, have higher BMD than Asians. Moreover, peak BMD among Asian women (Chinese and Japanese) is also substantially lower than Caucasian women. We previously noted that peak BMD in Vietnamese women and men was ~9% and 7% lower than Caucasian women and men, respectively.
The difference in peak BMD between Asians and Caucasians has major implications for the diagnosis of osteoporosis. An Asian woman may be diagnosed with osteoporosis based on the NHANES III reference range, but non-osteoporosis on an Asian reference range. Indeed, a study in a Chinese population revealed the prevalence of osteoporosis in women based on the NHANES III data (14.5%) was 3 times higher than that based on Asian reference range provided by GE Healthcare. The same difference was also observed in Chinese men among whom T-scores derived from the NHANES III reference range overestimated the prevalence of osteoporosis more than 3-fold, when compared with the Asian reference range.
Our population based study in Vietnam found that in women aged 50+ years, using the NHANES III reference range, the prevalence of osteoporosis was 44%, but if the local reference range was used, the prevalence would reduce to ~29% — which is incidentally, the same as the expected prevalence for the threshold of -2.5 as mentioned above. Moreover, in men aged 50+ years, the prevalence of osteoporosis based on the Vietnamese reference range was 10%, about one-third of the prevalence based on the NHANES III reference range.
In summary, it is clear from the above studies that the use of NHANES III reference range can result in a substantial overdiagnosis of osteoporosis in Asian women and men. The overdiagnosis can potentially lead to unnecessary anxiety for patients and overtreatment. If the NHANES III reference range is to be used for diagnosing osteoporosis in Asian women, an adjustment seems appropriate.
It can be argued that the application of the T-score threshold of -2.5 to Asian populations is not evidence based. Due to the lack of prospective data, it’s not known whether the lifetime risk of fracture in Asian populations is the same as in Caucasian populations. It is also not known whether Asians have the same absolute risk of fracture as Caucasians for the same level of BMD. We need more research to address those gaps in knowledge.
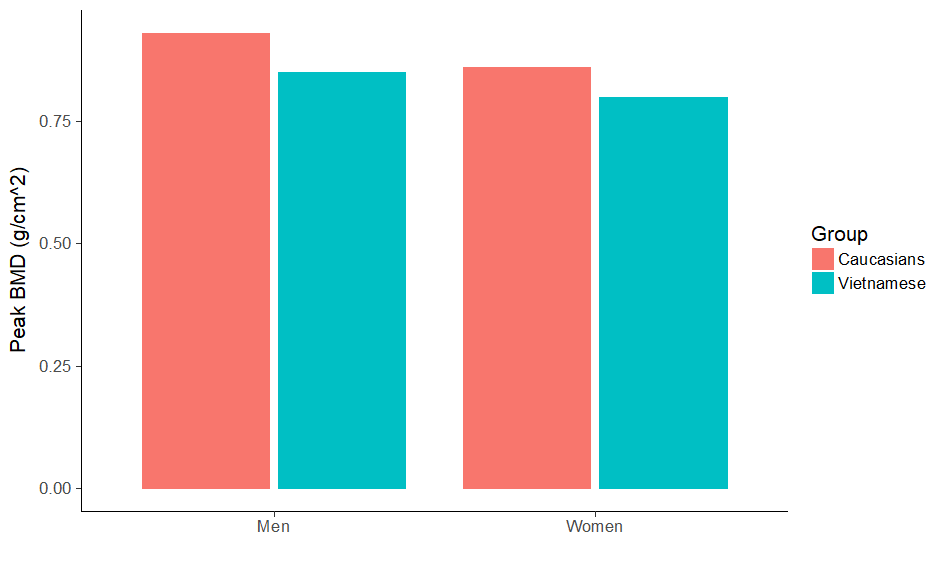
Peak bone mineral density in Vietnamese and Caucasian (NHANES III). Data are shown for femoral neck BMD measured by Hologic Horizon. Adapted from Ho-Pham et al, BMC Musculoskelet Disord. 2011;12:182.
Professor Tuan V. Nguyen, Garvan Institute of Medical Research, Sydney, Australia.