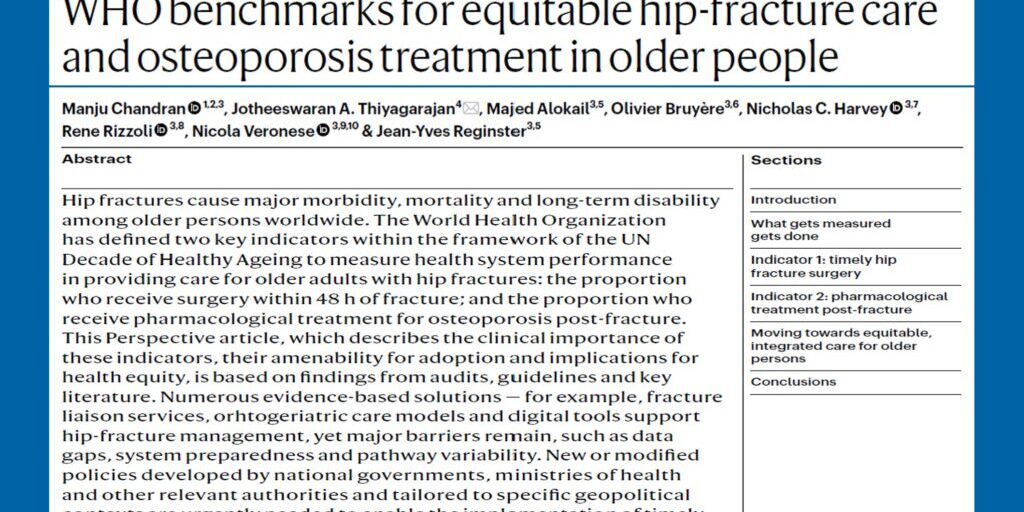
Progressive bone mineral density (BMD) loss due to oestrogen deficiency in postmenopausal women is a key factor in ‘osteoporotic’ or ‘fragility’ fractures, with approximately 50 per cent of post-menopausal women experiencing at least one fracture after the age of 50.1 Due to the rapidly ageing global population, we are seeing an increasing trend in the number of people being impacted by fragility fractures, which can ultimately place a heavy burden on quality of life.
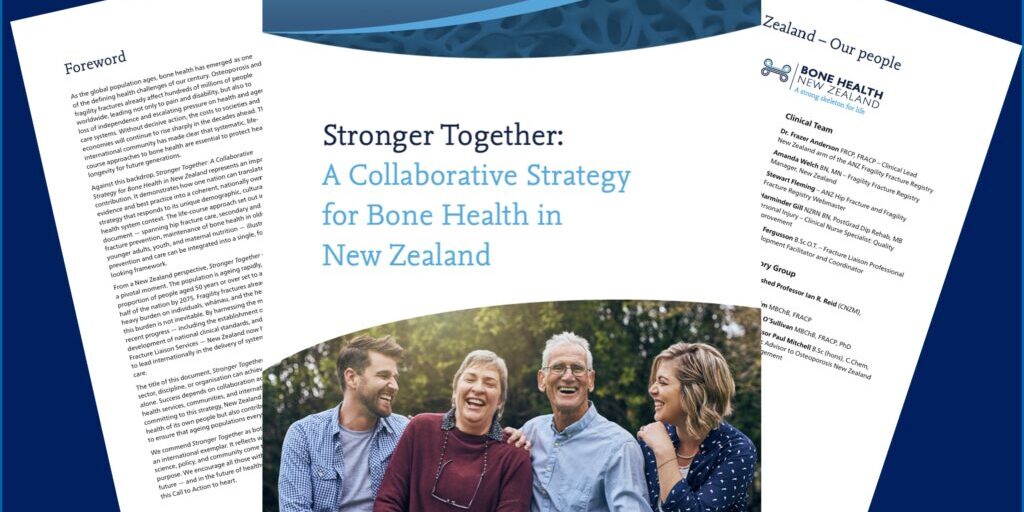
According to a recent perspectives piece published in Nature Reviews Endocrinology by Head of Department of Medicine, University of Auckland and APCO member, Professor Ian Reid, New Zealand, alarming discrepancies exist between the number of postmenopausal women currently being recommended for anti-fracture interventions, and those from the same demographic who have sustained at least one bone fracture,2,3,4 reinforcing the need for a broader, more inclusive strategy for osteoporosis intervention.
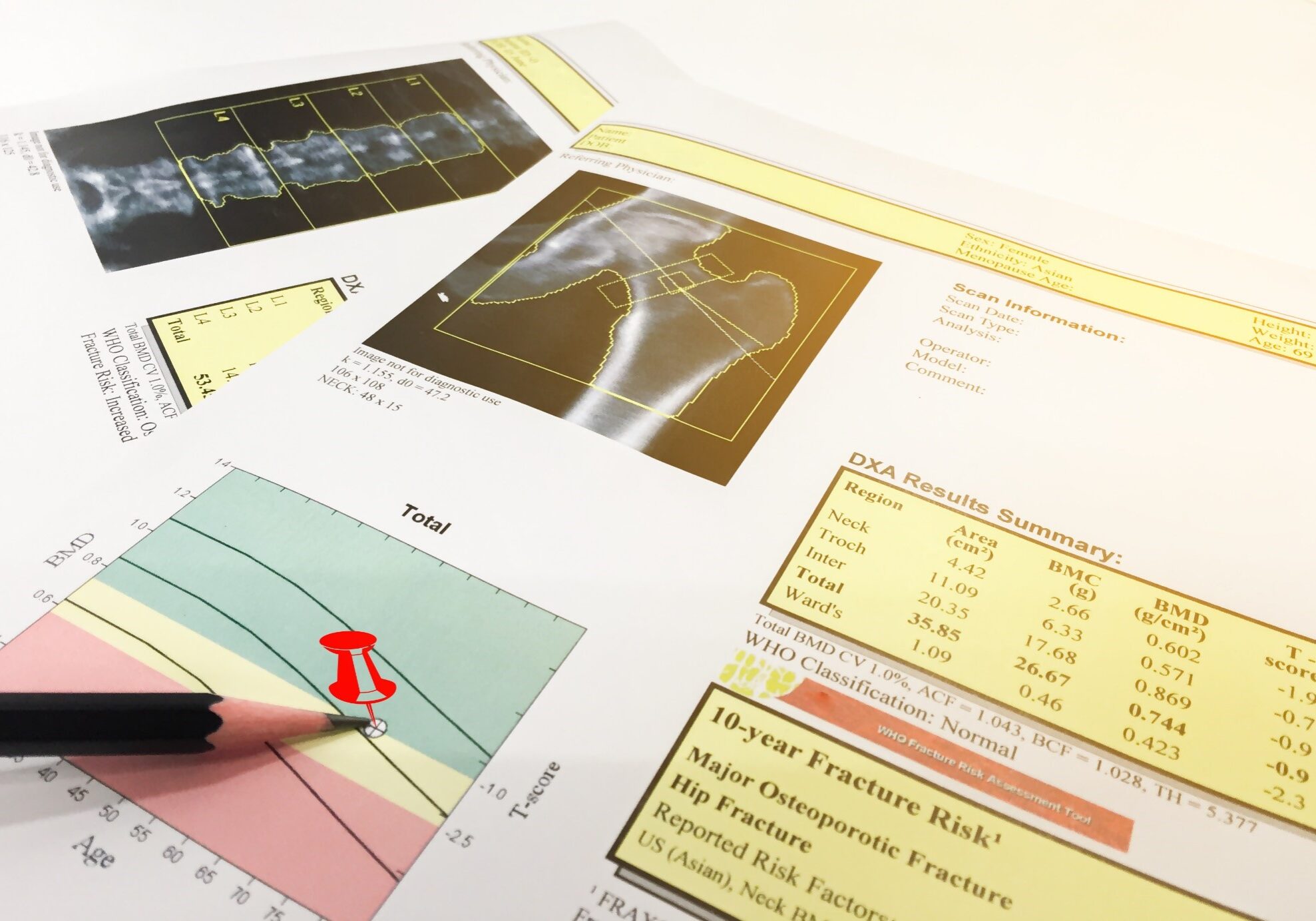
In many countries, the current approach to osteoporosis management for this vulnerable group constitutes screening women aged over 60 using clinical risk factors, and in some cases, measurements of BMD. Anti-fracture interventions are targeted to those considered at highest risk of osteoporotic fractures.5,6,7,8
With increased life expectancy being a notable trend over the past few decades worldwide, the number of women who are at risk of osteoporosis and the number of fractures sustained as a consequence is snowballing across the globe. Despite concerning statistics on the increasing prevalence of osteoporotic fractures, evidence shows anti-fracture interventions, such as anti-resorptive therapies, are currently only being recommended in seven to 25 per cent of women screened, falling significantly short of the number likely to experience a fragility fracture.2,3,4 Moreover, these recommendations are only being implemented/actioned in six to 18 per cent of cases,2,3,4 indicating current osteoporosis intervention criteria do not identify a large enough proportion of those who will experience a fracture, in order to substantially impact on the number of fractures sustained.
While existing osteoporosis intervention criteria, such as femoral neck BMD scores, are predictive of fractures, it is important to note osteoporosis, as defined by a BMD of >2.5 standard deviations below the mean value in the young population (that is, a T-score of <–2.5), characterises only about 20 per cent of older women who break bones.9 In Australia, approximately eight in 10 fractures sustained in older women, occur in those who are not classified as being osteoporotic, as measured by BMD.10
Similarly, commonly used risk thresholds, including BMD, FRAX and a combination of criteria proposed by The National Osteoporosis Foundation (NOF), only identified 3 to 30 per cent of women aged 60 to 69 years and 15 to 56 per cent of those aged 70 to 79 years, as meeting the criteria for intervention.11 Therefore, most women who had sustained fractures during follow-up were not identified as being at risk, using the thresholds considered in this analysis.
While evidence suggests most of the current osteoporosis intervention criteria do not sufficiently identify the number of people who will experience a fracture, the same assessment methods could potentially continue to be used with different thresholds for intervention.
For example, one study indicates using a BMD T-score of -1 would enable treatment of 80 per cent of those who would subsequently fracture.12 However, the cost and benefits of this approach would need to be considered, as this would require treating many individuals who would not sustain a fracture.
Treatment strategies involving a broadening of anti-fracture interventions could offer a solution for capturing a larger pool of the at-risk population. Studies investigating this approach, conducted over the past 15 years, have all shown substantial reductions in the number of fractures sustained.13,14,15,16,17,18,19
In broadening the scope of anti-fracture intervention, it would be pertinent to consider other factors when qualifying postmenopausal women with a low-to-moderate risk of osteoporotic fracture, for treatment. Such factors include cost, adherence and, above all, safety.
The cost of broadening anti-fracture interventions to a much larger population means this strategy is only feasible for generic medications. Given the low cost of generic bisphosphonate medicines in most countries, this should not be a limiting factor.9
Adherence to a prescribed intervention in low risk populations is frequently considered a hurdle. However, the long duration of action of some anti-fracture interventions makes intermittent therapy possible, which may serve to negate the repercussions of low treatment adherence.18
Safety should always be of greatest concern when considering a broader approach, particularly in the widespread use of anti-resorptive therapies, which have been linked to osteonecrosis of the jaw (ONJ)20,21 and atypical femoral fracture (AFF).22 While this is a legitimate concern that should be considered for every individual case, the findings of a 2018 clinical trial of osteopenic postmenopausal women showed no AFFs in the treatment group, and a substantial reduction in other fracture types, suggesting fractures prevented overall, overwhelmingly outweigh the potential adverse events.18
In a bid to close the gap between postmenopausal women experiencing fractures, and those recommended for intervention, revised guidelines are warranted to proactively identify a broader range of suitable candidates for anti-fracture management.
For the Asia Pacific region, home to more than a third of the world’s population aged 65 years and over, and to more older people than any other region,23 these considerations are even more pertinent.
The Asia Pacific Consortium on Osteoporosis (APCO), comprising osteoporosis experts from several countries in Asia Pacific, is charged with developing tangible solutions to the substantive challenges involving osteoporosis management and fracture prevention in this most populated and fastest growing region of the world.