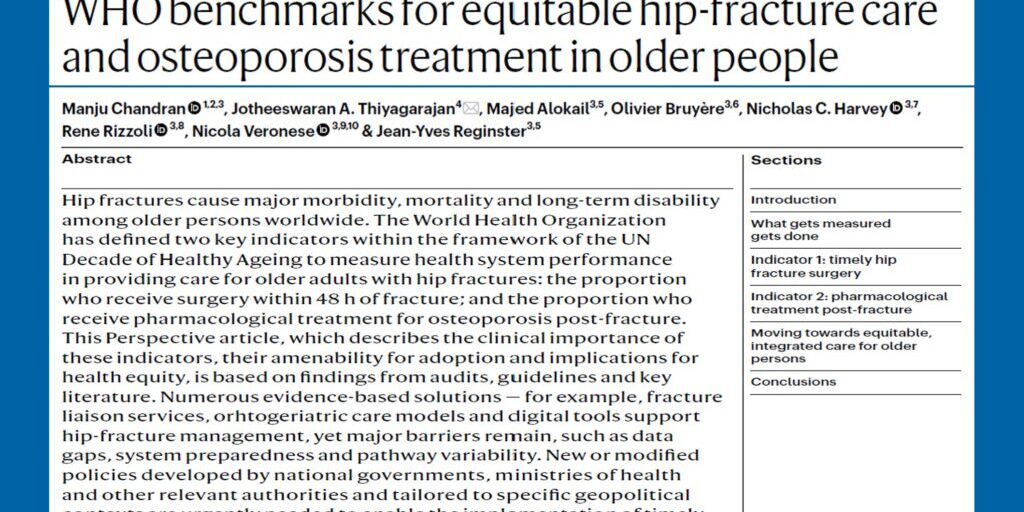
The number of individuals at risk for fragility fractures worldwide is predicted to increase two-fold from the 158 million it was in 2010, to 319 million in 2040. This grave projection is going to be felt most keenly in Asia; home to 4.5 billion people and to several rapidly aging societies.
The financial costs associated with the treatment of osteoporosis and osteoporotic fractures is huge. However, how can limited health care resources be efficiently allocated to osteoporosis? Who decides on this allocation and what should form the basis for this allocation? How do we derive cost -effective thresholds for osteoporosis treatment and can a uniform intervention threshold be used for the entire Asia Pacific region? The answer to the latter question is obviously an emphatic No. Intervention thresholds in osteoporosis will vary, since they depend critically on country-specific factors such as reimbursement and cost issues, willingness to pay for healthcare, and access to medications and bone mineral density testing. Significant heterogeneity in epidemiologic, ethnographic, and economic characteristics and access to resources exist between the countries that make up the vast expanse of the Asia Pacific region. Therefore, it is quite clear that intervention thresholds should be country- specific. It is also clear that these intervention thresholds should not only be clinically appropriate for, but also must be cost-effective in the country that it is being implemented in. It cannot and should not be assumed that intervention thresholds that are cost-effective in one country will equally be cost-effective in another.
Health economic analysis is playing an increasingly important role to inform the relative value of osteoporosis therapies and to help determine how best to intelligently allocate finite health care resources. The development of absolute fracture risk-based assessment and intervention thresholds has led to the exploration of cost-effectiveness of interventions along the lines of fracture probability with either fixed, or age-dependent intervention thresholds being evaluated by different investigators.
A FRAX®-based fixed hip fracture intervention threshold of 3% and a major osteoporotic fracture intervention threshold of 20% were deemed as cost-effective from a health economic analysis done more than a decade ago in the USA. These specific thresholds have somehow found their way to being adopted without question in several other parts of the world. Age-dependent thresholds have been found to be cost-effective in the UK and, the National Institute for Health and Care Excellence (NICE) of the United Kingdom’s updated Multiple Technology Appraisal (MTA) on bisphosphonate use in osteoporosis concluded that generic oral bisphosphonates were cost effective for people with even a 1% major osteoporotic fracture risk. In contrast, a recent study from Singapore using a previously validated economic model adapted to the Singapore context showed that treating post-menopausal women with generic alendronate was cost-effective only at a much older age than what was noted in the UK. The fixed thresholds that were identified to be cost-effective were also different from that noted in other countries. Outside the one done in Singapore, robust health economic evaluation studies in osteoporosis are few in the Asia-Pacific region. Those that have been done have employed different modelling strategies. Varying results have been obtained from these studies and they highlight the crucial differences in economic, epidemiological, and even clinical practice processes and factors between the countries in the vast region that is the Asia-Pacific. They also highlight the important fact that the kind of intervention thresholds that can be utilized in an Asian country are not necessarily the same as what can be employed in a country in the west. One size indeed does not fit all when it comes to osteoporotic treatment thresholds.
The Framework of Minimum Clinical Standards of Care being developed by the Asia Pacific Consortium on Osteoporosis (APCO) emphasises the need for countries in the Asia Pacific region to develop country-specific, cost-effective intervention thresholds for the management of osteoporosis whilst still adhering to the minimum standards of care advocated in the Framework.
Dr Manju Chandran, Senior Consultant and Director, Osteoporosis and Bone Metabolism Unit, Singapore General Hospital and Chairperson, Asia Pacific Consortium on Osteoporosis (APCO) and Mickaël Hiligsmann, Associate Professor in Health Economics and Health Technology Assessment at Maastricht University, the Netherlands.