Dr Nigel Gilchrist, Canterbury District Health Board, Christchurch, New Zealand and APCO Executive Committee Member
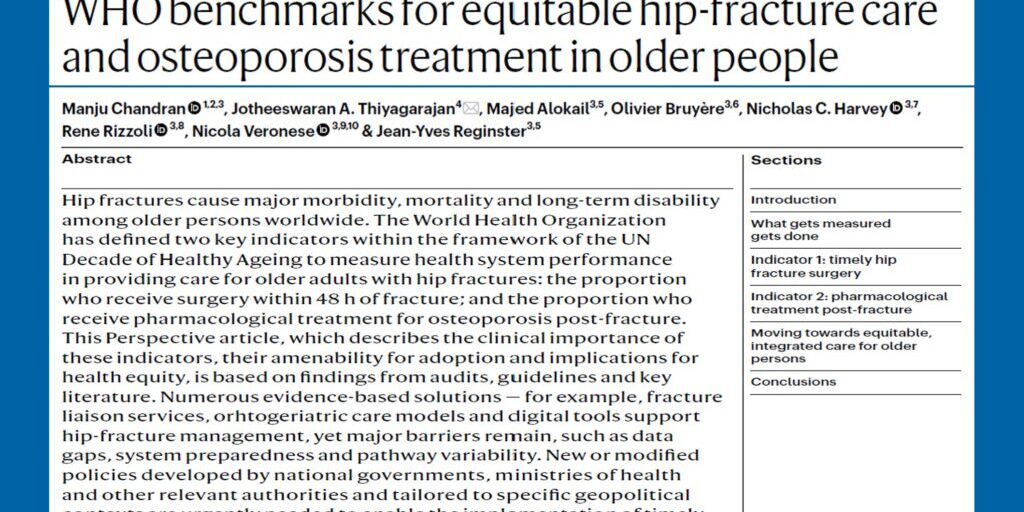
Hip fractures in old adults are common, affecting up to 18 per cent of women and 6 per cent of men in their lifetime, and are associated with significant mortality and burden of disease. In the setting of prompt surgery and orthogeriatric care rehabilitation, approximately 10 per cent of patients will experience a second hip fracture which will further negatively impact their mortality and quality of life. In our area, the older population is increasing now, representing up to 16 per cent of the total population.
We are based in a large tertiary hospital, the busiest trauma hospital in New Zealand. Following hip fracture, older patients are cared for in a range of settings, with input from both geriatric and orthopaedic specialists. We have a shared care model that manages patients, comorbidities, and rehabilitation. Patients may be offered rehabilitation, or discharged to other locations. We have recently examined the characteristics and treatment outcomes and rehabilitation practices for this group of patients with hip fractures. We are fortunate in our institution of being able to access multiple data sets for analysis. The four groups we examined were:
- Publicly funded aged residential care residents who were discharged from acute orthopaedics;
- Those directly discharged home;
- Patients discharged after specific orthogeriatric rehabilitation; and
- Patients discharged after general geriatric rehabilitation.
We aimed to compare these groups, by focusing on length of stay, comorbidity, functional status and treatment for osteoporosis.
In the past we have implemented a fast-track management system for hip fracture management. In comparison with this previous work, it is showing that our wait for surgery has decreased, with most people undergoing an operation within 48 hours, with no difference in wait for surgery between the four groups. Notably, over a quarter of these patients had a prior hospital admission for fracture, and 43 per cent had experienced a hospital admission for other reasons within one year of their hip fracture.
Mortality was highest among the aged care residents who were discharged from acute orthopaedics. The 30-day in hospital mortality was 10 per cent, and the longer 6-month mortality was 7 per cent in the orthopaedic rehabilitation group, and 8 per cent in the general rehabilitation group. Length of stay was shorter in the orthogeriatric rehabilitation group at 12.9 days, but longer in the general rehabilitation group, at 20.4 days, reflecting the level of other comorbidities.
We also concentrated on the treatment for osteoporosis. We have a very active fracture liaison service (FLS) within our hospital systems, but all of the acute and rehabilitation wards have standard osteoporosis treatment guidelines. We found that 88 per cent of the patients in the orthopaedic rehabilitation group received appropriate treatment for osteoporosis, while in the general rehabilitation group, only 62 per cent did. The group that appeared to not receive ideal treatment for their osteoporosis were those discharged directly from the acute orthopaedic wards (i.e., going to other hospitals or other regions), with treatment rates varying between 15 and 42 per cent.
Since this work we have instituted a mandatory field in the discharge letter from acute orthopaedics, and FLS has targeted this group. This work has shown that patient outcomes have generally improved, and identification and treatment for osteoporosis has significantly improved. This work further supports consideration of a randomised trial to examine the effects of targeted post-surgical rehabilitation with hip fractures, and explore measures to increase the uptake of osteoporosis treatment.