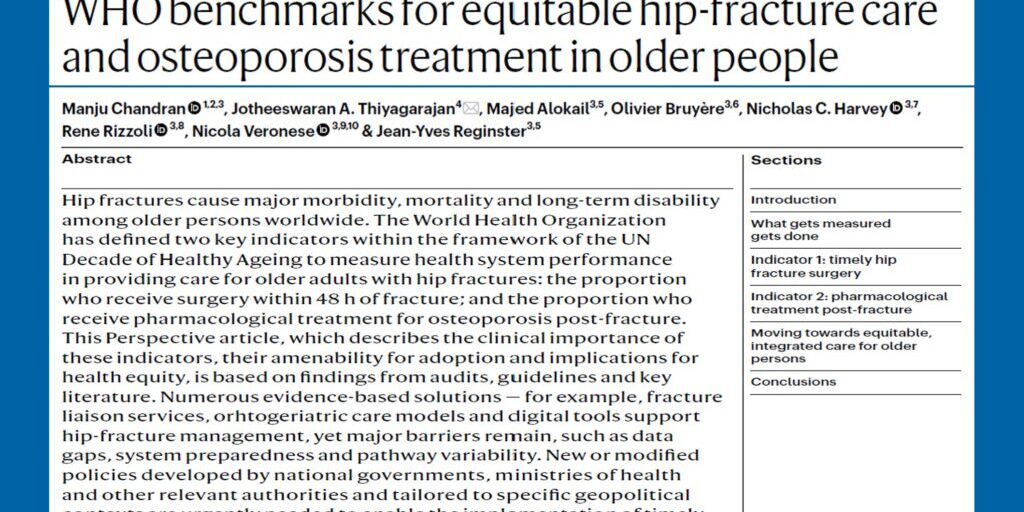
An article written by Asia Pacific Consortium on Osteoporosis (APCO) Executive Committee Chair, Dr Manju Chandran and APCO Executive Committee member and Medical Director of Osteoporosis Australia, Professor Peter Ebeling AO titled ‘Osteoporosis management and fracture prevention’, has just been published in the Medical Journal of Australia’s (MJA) online peer-reviewed publication, MJA Insight, which is amongst the world’s top 20 general medical journals.
The article highlights the burden of osteoporosis in Australia and the Asia Pacific, and outlines the steps to be taken to ensure better bone health for the region. The article further reinforces the importance of secondary fracture prevention and how it can be achieved through two key strategies – the development and implementation of evidence-based osteoporosis management guidelines and the funding and implementation of fracture liaison services (FLS).
The article outlines APCO’s mission, purpose and ‘Framework’, and the consortium’s role as a “catalyst for ideas and an enabler for individuals in the health care arena who are committed to osteoporosis care, to bring about change in the Asia Pacific region, with regard to osteoporosis care and management.” Australia has a very important role in APCO. It hosts APCO’s administration within Osteoporosis Australia and has contributed the recent 2017 RACGP/OA guidelines for osteoporosis management to the development of the APCO Framework.
See below for the introductory paragraphs to the MJA Insight article. To read the full article, head here.
Osteoporosis is a chronic disease associated with ageing and is increasing in Australia and the Asia Pacific. The Asia Pacific, home to more than half of the world’s population, is ageing rapidly. The age structure of this population is set to undergo an unprecedented demographic shift in the coming decades, resulting in the proportion of individuals who will be aged 65 years and over increasing several-fold, as compared with younger working-age individuals. Maintaining the mobility of these older individuals and, therefore, their independence, will allow nations and their policymakers to adjust to the realities of this new demographic era by reducing hospitalisations.
Prevention of osteoporosis and falls – and subsequent fragility fractures – must be recognised as a health care priority throughout the Asia Pacific. More than 1.2 million Australians have osteoporosis, with about 24 000 hip fractures occurring each year (here and here), which is projected to cost $1.13 billion per annum by 2022 (here and here). By contrast, projections for hip fractures in the Asia Pacific dwarf this number. In 2018, more than 1.1 million hip fractures were anticipated to occur in nine countries or regions in the Asia Pacific, incurring an estimated direct cost of US$7.4 billion.
However, by 2050, the number of hip fractures will more than double to more than 2.5 million cases annually, resulting in projected costs of almost US$15 billion by 2050 and comprising over 50% of the world’s hip fractures. Notably, China sustained 43.1% of the region’s hip fractures in 2018, but incurred just 22.7% of the costs, while Japan sustained 15.9% of the hip fractures, but incurred 66.4% of the costs. However, a recent update revealed the Chinese costs were conservative, and are likely to be more than double based on more recent estimates. This demographic change is the reason international organisations, such as the International Osteoporosis Foundation (IOF), are focusing on this region for preventive strategies, for which some Australian initiatives could provide a good model.
Read more here.