Practical tool kit promoting quality improvement of osteoporosis care to avoid the dreaded consequence of fragility fractures that can cause pain, long-term disability, & loss of independence
The Asia Pacific Consortium on Osteoporosis (APCO) has launched a Bone Health QI Tool Kit today (May 24, 2022), to address the major public health burden of osteoporosis throughout the Asia Pacific (AP).
A world-first of its kind, the tool kit aims to promote quality improvement (QI) in osteoporosis care in a bid to stem the current crisis in osteoporosis care. It is based on seven selected standards from the APCO Framework that are applicable to the clinical setting. Previous audit tools have focused on mostly one aspect of osteoporosis care, namely the identification and management of osteoporotic fragility fractures, while the APCO tool kit targets multiple components in the screening, diagnosis, and management of osteoporosis.
Implementation of QI will be through Plan-Do-Study-Act (PDSA) cycles.
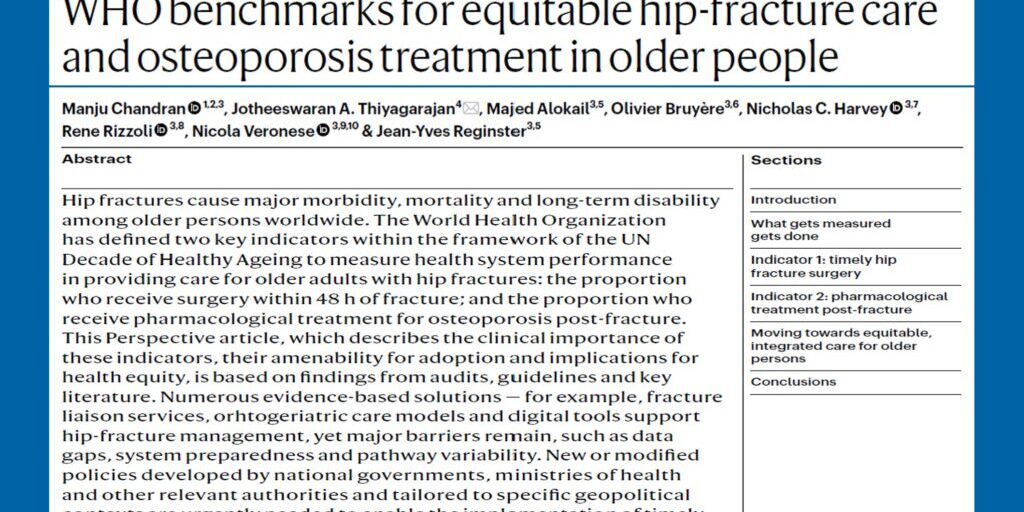
Currently one-in-four patients who sustain a hip fracture die within a year, and less than half of those who survive, regain their previous level of function. The expected direct incurred cost associated with the more than 1.1 million hip fractures estimated to have occurred in nine countries and regions in the AP, including China, Chinese Taipei, Hong Kong SAR, India, Japan, Malaysia, Singapore, South Korea, and Thailand in 2018, amounted to USD 7.5 billion. Concerningly, this cost is projected to increase to almost USD 13 billion by 2050.
In a bid to help close this care gap, the APCO Bone Health QI Tool Kit focuses on:
- Understanding the baseline variables and current state of osteoporosis care in any given institution or health care practice.
- Enabling benchmarking clinical practice against the APCO Framework, evidence-based clinical practice guidelines, or other established protocols for the chosen standard of care.
- Using the findings to then improve the quality of care through iterative PDSA cycles.
- Using the lessons learned from implementation of the QI project at an institutional level, to build momentum, and work towards inclusion of the quality improvement/clinical standard in national guidelines, and lobbying for funding and policy change, as appropriate.
Practically, PDSA cycles are a quality improvement strategy that tests a change on a small scale. The PDSA builds on the learning from these test cycles in a structured way before implementation on a wider scale.
The PDSA cycles are iterative. Each cycle involves four stages:
- Plan – developing a plan to test the change;
- Do – carrying out the test;
- Study – observing and learning; and
- Act – planning the next change cycle or full implementation.
“A perfect storm of a rise in osteoporosis among Asia Pacific populations is expected to occur due to the
region’s rapidly aging population, mounting urbanisation, and subsequent increase in sedentary lifestyles,” explained Dr Manju Chandran, APCO Chairperson and Director of the Osteoporosis and Bone Metabolism Unit, Singapore General Hospital, Singapore.
“In fact, a recent analysis of nine Asian countries and regions reveals the number of hip fractures will more than double from 1.13 million in 2018, to 2.54 million in 2050,3 primarily due to changing population demographics.
“Once the Bone Health Audits are completed, healthcare professionals and medical centres can embark on implementing changes to their clinical practice,” Dr Chandran said.
“APCO is currently in the process of engaging QI experts to help train APCO members to conduct such projects in their individual medical centres and practices.”
By 2050, one in four people in AP will be aged over 60 years. This portion of the population is expected to triple between 2010 and 2050, reaching close to 1.3 billion people. Within the same timeframe, between 4.5 to 6.3 million hip fractures are predicted to occur worldwide, half of which will occur in Asia.
The likelihood of successfully creating change to stem this crisis depends largely on the success of HCPs in engaging their peers to work towards shared goals, said Dr Philippe Halbout, CEO, International Osteoporosis Foundation (IOF), Switzerland, and APCO Executive Committee Member.
“Osteoporosis is greatly under-diagnosed and under-treated in Asia, even among those at highest risk who have already fractured.
“Lessons from implementing these clinical standards at the institutional level will be key to achieving change at the national level, through the development or revision of national guidelines, and for driving policy change,” Dr Halbout said.
“These coordinated systems of care aim to identify, treat and monitor patients presenting with a fragility fracture. Intervention can reduce fractures by up to 50 per cent, deliver substantial financial savings, and ultimately, save lives.”
To learn more about the APCO Bone Health QI Tool Kit, visit www.apcobonehealth.org or follow APCO on LinkedIn: asia-pacific-consortium-on-osteoporosis.