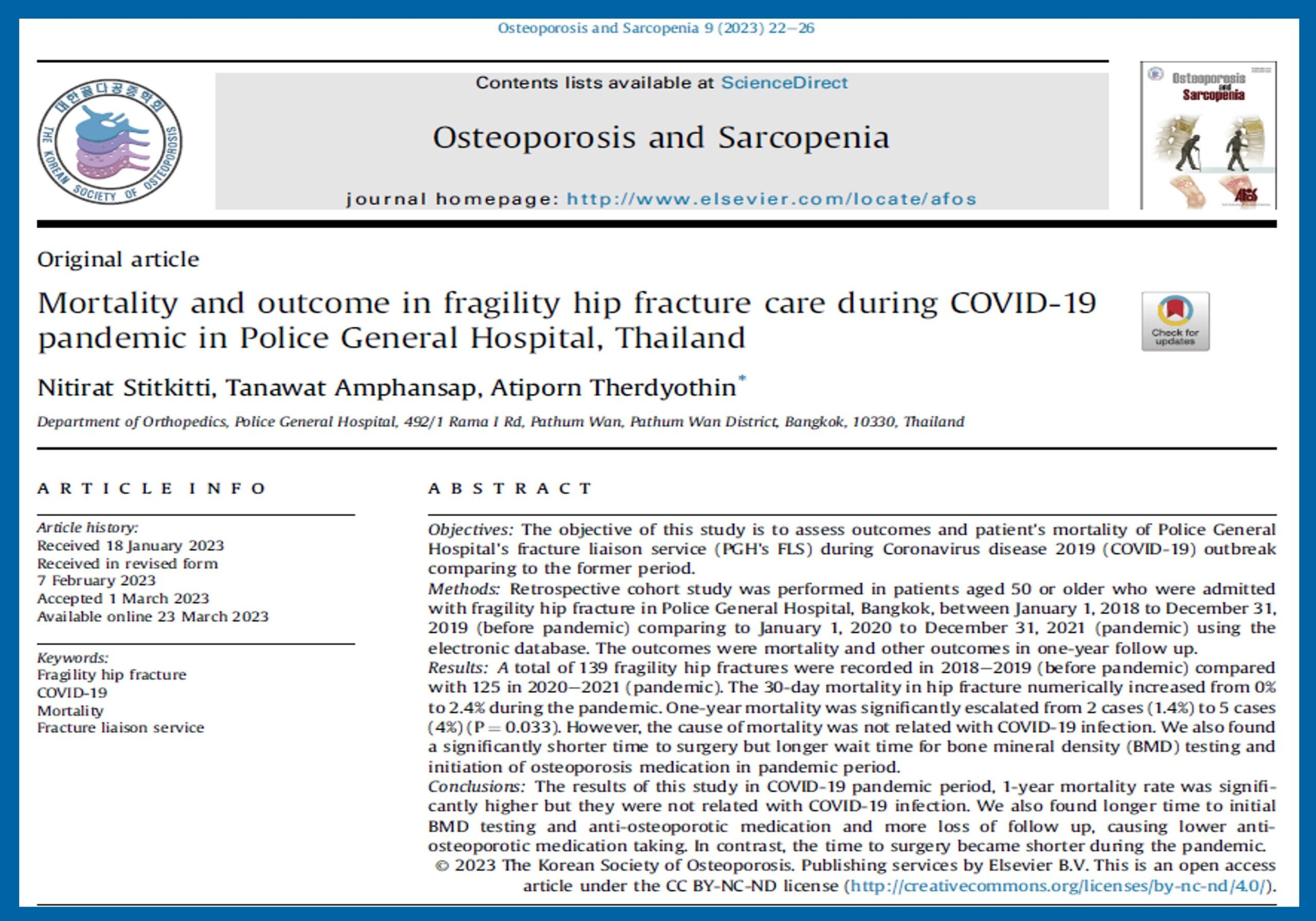
Researchers from Police General Hospital’s (PGH) Fracture Liaison Service (FLS) in Bangkok, Thailand, collaborated recently to consolidate and analyse data on the outcomes and mortality rates of patients with osteoporotic hip fractures at their centre during the Coronavirus Disease 2019 (COVID-19) pandemic compared to the period before the outbreak. The review was published in the March 2023 issue of the journal – Osteoporosis and Sarcopenia. The retrospective cohort study was conducted using data obtained from PGH’s FLS registration database from the period of January 1, 2018, to December 31, 2021.
The article had as its lead authors, APCO member, Dr Tanawat Amphansap, and his colleagues Dr Nitirat Stitkitti and Dr Atiporn Therdyothin from the Department of Orthopaedics at the Police General Hospital, Thailand. The retrospective cohort study was performed in patients aged 50 or older who were admitted with fragility hip fracture in PGH between January 1, 2018, to December 31, 2019 (before the pandemic) compared to January 1, 2020, to December 31, 2021 (pandemic) using data procured from the electronic database of the hospital. Mortality at one year follow-up and other outcomes such as time for Bone Mineral density (BMD) testing and to osteoporosis treatment initiation were evaluated.

When comparing pre-pandemic (2018-2019) to the pandemic (2020-2021) data, the researchers found a significant increase in one-year mortality from 1.4% to 4%. The cause of mortality appeared to be not directly related to COVID-19 infection. The research also revealed noteworthy changes in the treatment timelines during the pandemic. The time to surgery for hip fractures became shorter. The higher operative rate during the pandemic was attributed to more available operative rooms as elective surgery was postponed to avoid COVID-19 infection. It was also likely due to more patients opting for riskier surgery as compared to conservative treatment to reduce their time of stay for treatment at the hospital. However, because the pandemic also saw the diversion of healthcare personnel to cope with the increase of patients with COVID-19 infection available slots for physiotherapy and testing were less. Therefore, the wait time for bone mineral density (BMD) testing and initiation of osteoporosis medication increased significantly.
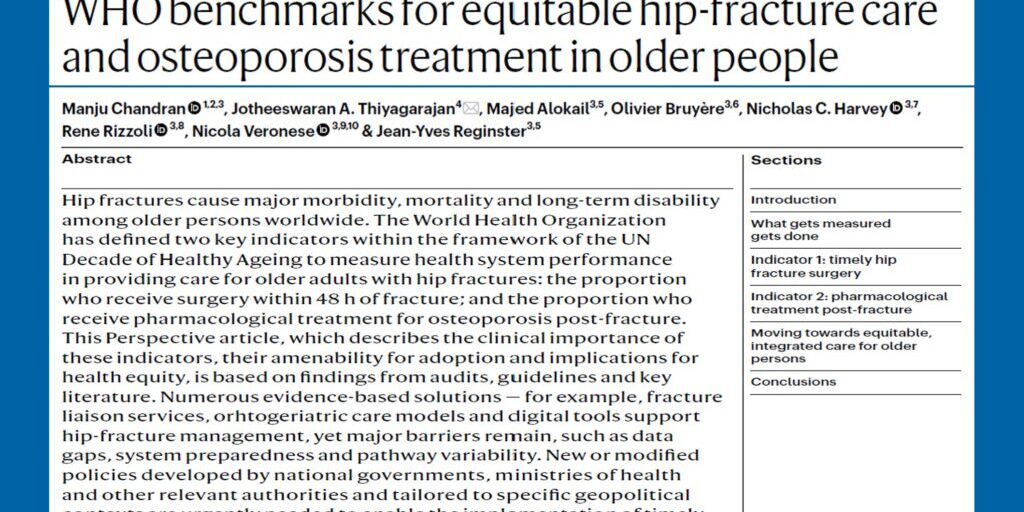
The investigators discuss how the increase in mortality noted during the period studied could be partially explained by the limited number of healthcare personnel, and delayed contact with healthcare providers. The authors also discuss how the implementation of FLS in their institution (PGH) has resulted in a reduction in mortality rate as compared to other institutions of similar size.

The authors recognize the need for new initiatives to improve patient care and improve the outcomes and mortality rates of patients with osteoporotic hip fractures. In the review, the authors explain new initiatives they have introduced at their institution and discuss the impact they have had. The authors acknowledge the several limitations of this study such as not assessing other outcomes like post-operative functional outcome or quality of life.
The research team believes that the findings from this study could have significant implications for hospitals and healthcare providers during this challenging period. Further research is recommended to delve deeper into the reasons behind the observed changes in mortality rates. Adjustments in healthcare deliveries are needed to reach more patients during inevitable future pandemics and the new-normal scenario
To read the full text of the article, click here.
Reference:
Stitkitti N, Amphansap T, Therdyothin A. Mortality and outcome in fragility hip fracture care during COVID-19 pandemic in Police General Hospital, Thailand. Osteoporos Sarcopenia. 2023 Mar;9(1):22-26. doi: 10.1016/j.afos.2023.03.001. Epub 2023 Mar 23. PMID: 37035092; PMCID: PMC10034845.