The bone loss and increased bone fragility that results from specific, well-defined clinical disorders, and due to certain medications, is termed secondary osteoporosis. Pre- and post-menopausal women, as well as men, may develop secondary osteoporosis. Up to 45% of post-menopausal women, and 60-65% of men are found to have an underlying contributor to their osteoporosis on evaluation.
Myriad medical conditions may cause bone loss and increased skeletal fragility. They include endocrine disorders (hypogonadism, Cushing’s syndrome, primary hyperparathyroidism, diabetes mellitus), gastrointestinal disorders (celiac disease, inflammatory bowel disease, lactose intolerance, chronic liver disease), hematological disorders (multiple myeloma, monoclonal gammopathy of undetermined significance, systemic mastocytosis), renal disorders (chronic kidney disease, renal tubular acidosis), autoimmune disorders (rheumatoid arthritis, systemic lupus erythematosis) etc. The use of certain medications (glucocorticoids, aromatase inhibitors, thiazolidinediones, etc.) is also associated with secondary osteoporosis.
Secondary osteoporosis should always be suspected in pre-menopausal women and younger men presenting with low bone mass and / or fragility fractures. Clinical suspicion of secondary osteoporosis should be high, even in older men and post-menopausal women.
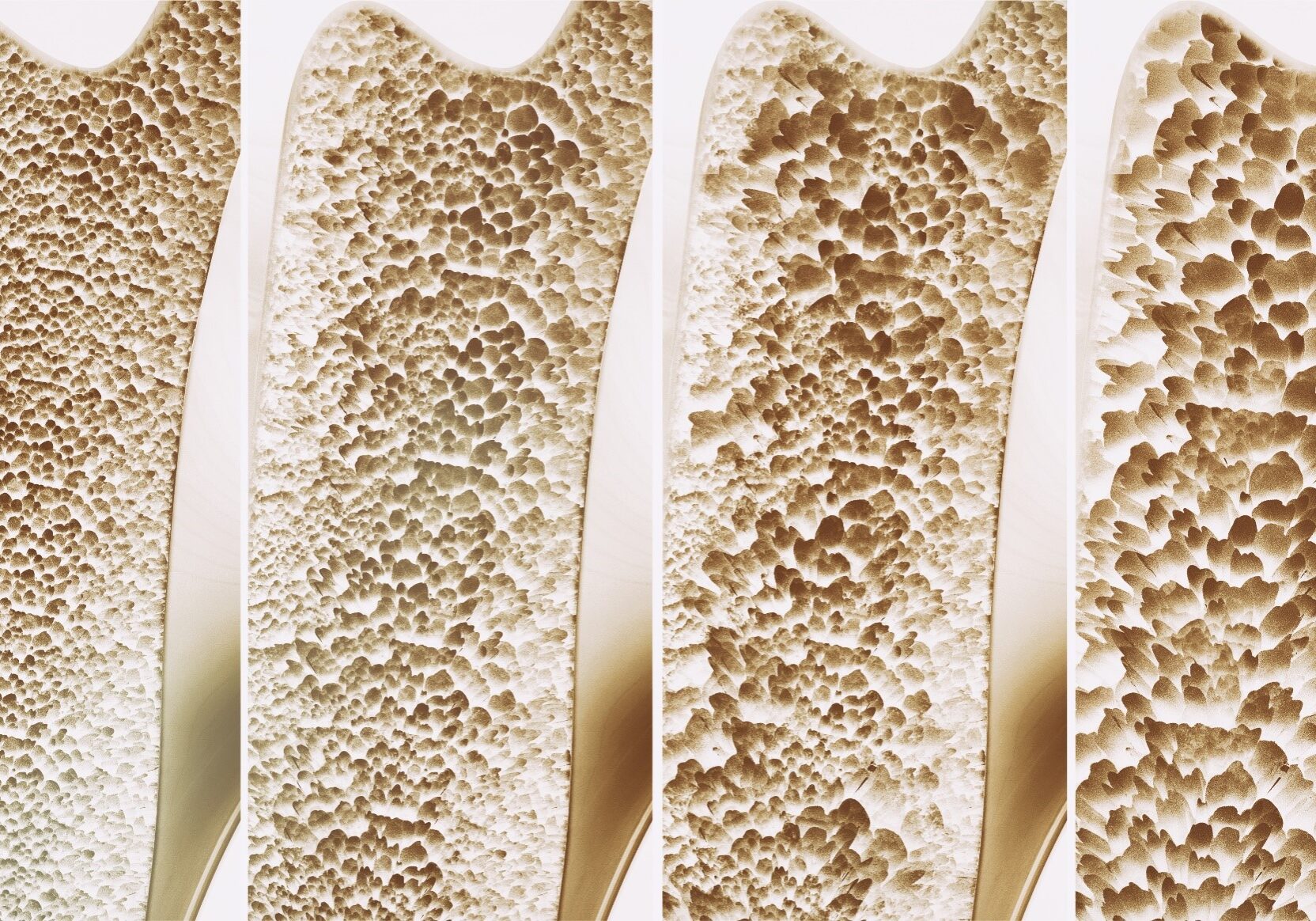
No definite threshold of BMD Z-scores have been found to rule in or rule out secondary osteoporosis. Work-up should begin with a detailed history and a thorough physical examination. Preliminary biochemical investigations include measurement of serum calcium, phosphate, albumin, total alkaline phosphatase, creatinine, 25-hydroxvitamin D, parathyroid hormone, thyroid function tests and complete blood count. Subsequent work-up must be guided by the initial evaluation and could include estimation of serum gonadal hormones, luteinizing hormone, prolactin (for hypogonadism), cortisol dynamics (for Cushing’s syndrome), fasting/post-prandial blood glucose, glycated hemoglobin (for diabetes mellitus), serum protein electrophoresis (for multiple myeloma), IgA tissue transglutaminase antibody (for celiac disease), blood-gas analysis (for renal tubular acidosis) and anti-nuclear antibody / rheumatoid factor (for autoimmune diseases). The validity of areal BMD as a predictor of incident fractures is not well established in patients with secondary osteoporosis. Fractures may occur even at a reasonably normal BMD, as in patients with glucocorticoid-induced osteoporosis (GOI) and Type 2 diabetes mellitus, limiting the value of BMD in these patients. Such patients tend to have deterioration of bone microarchitecture that is not picked up on areal BMD. Instead, the physician can contemplate the use of volumetric BMD and trabecular bone score while evaluating a patient with secondary osteoporosis. Instead of the routine BMD-based FRAX, TBS-adjusted FRAX score can be a better predictor of incident fractures in such patients.
Management of secondary osteoporosis involves treatment of the underlying cause (gonadal hormone supplementation in hypogonadism, control of hypercortisolism in Cushing’s syndrome, excision of parathyroid adenoma in hyperparathyroidism, gluten-free diet in celiac disease, etc.). Calcium and vitamin D supplementation should also be continued as in patients with primary osteoporosis. When a medication is identified as responsible for the bone loss, all efforts should be made within the realm of reason to use the lowest possible dose of the medication, as in the case of glucocorticoids, so as to reduce the risk of bone loss and subsequent fracture risk. In addition, available anti-osteoporotic medications (anti-resorptives or anabolics) can be used in patients with secondary osteoporosis.
Professor Sanjay K. Bhadada, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India and APCO Executive Committee Member.